Ever felt like you’re standing at the crossroads of health care decisions, peering into the foggy intersection of Medicare and HSA? You’re not alone. The complex world of healthcare expenses and tax advantages can often feel as if we’ve stepped foot in a labyrinth.
“Do I go left towards Medicare enrollment? Or do I veer right to maximize my Health Savings Account (HSA) contributions?” Such questions echo around these puzzling pathways. But don’t worry! It’s time to shed light on this maze, map out your journey, and equip you with an understanding that will transform your decision-making process.
Let’s dive deeper into the tax impacts of HSAs and how enrolling in Medicare influences them. We’ll also explore situations where delaying Medicare might actually help with ongoing HSA contributions. This will give us a clearer picture of how to navigate these financial waters effectively.
Understanding Medicare and Health Savings Accounts (HSA)
Many Americans are anxious about their medical costs. This is where understanding the relationship between Medicare and HSA, or Health Savings Account, becomes crucial.
What is an HDHP?
A high-deductible health plan, often shortened to HDHP, has cheaper premiums but a greater deductible than standard insurance plans. These types of plans are relevant to HSAs because they qualify you for one. That’s right. You can’t just open an HSA; you need to have an HDHP first.
The idea behind this setup is simple: with reduced healthcare costs through lower premiums, people can set aside more money into their HSAs. This creates a sort of personal savings account for dealing with those unexpected medical bills that pop up now and then.
How does enrolling in Medicare affect your HSA?
The relationship between Medicare and HSA isn’t always clear cut. Here’s the deal – once someone enrolls in any part of Medicare (be it Part A or B), contributing pre-tax dollars to their HSA gets off-limits.
This rule applies even if only enrolled in Part A of Medicare which most folks get automatically when they start collecting Social Security benefits at age 65.source
You might wonder why anyone would want to delay such beneficial coverage? The answer lies within tax advantages offered by HSAs. If contributions to your HSA are made with pre-tax dollars, they reduce your taxable income. That’s a win-win situation for those high health care costs and keeping Uncle Sam happy.
Considering whether or not to postpone signing up for Medicare is a very personal choice. For example, if you have generous employer health coverage, it might make sense to hold off on Medicare and keep contributing funds into an HSA.
Figuring out the optimal approach can be complicated. But if you understand how HSAs and Medicare work together, you could potentially save some cash when handling your healthcare expenses.
Key Takeaway:
Mastering the dance between Medicare and Health Savings Accounts (HSA) can help ease your healthcare cost worries. Remember, you need a High-Deductible Health Plan to open an HSA, allowing for more personal savings towards unexpected medical bills. However, enrolling in any part of Medicare puts a stop to pre-tax dollar contributions into your HSA. But despite this drawback, it’s important to understand that balancing these resources is key to securing your health finances.
The Tax Implications of HSAs
HSAs, or Health Savings Accounts, come with some impressive tax benefits. Funds contributed to an HSA are not taxed when put into the account or when taken out for qualified medical expenses. That’s right. This money grows tax-free and can be used without any fear of Uncle Sam reaching into your pocket.
The Tax-Free Nature of HSAs
Contributions to an HSA offer triple tax advantages that few other savings accounts provide. First off, contributions reduce your taxable income for the year they’re made – it’s like writing off your future health care costs on this year’s tax return. Secondly, earnings from interest or investments in the account grow free from taxes as well.
Last but certainly not least is withdrawal; funds withdrawn for qualified medical expenses are also untaxed. So you get a deduction at deposit, growth without taxation over time and then withdrawals free from taxes if used properly – sounds pretty great.
Avoiding Tax Penalties When Enrolling in Medicare
If you’ve been contributing pre-tax dollars to an HSA before enrolling in Medicare, listen up: there could be a potential pitfall here related to timing that could trigger unexpected taxes.
You see, stopping HSA contributions at least six months before Medicare enrollment is necessary because when you sign up for Medicare Part A (hospital insurance), it comes with retroactive coverage extending back 6 months (but no further than the first month you were eligible). If during these past six months prior to enrollment if you continued making deposits into your HSA–boom–you may have just triggered a tax penalty.
But don’t fret. You can avoid this by simply stopping your HSA contributions 6 months before you apply for Medicare.
Monthly Adjustment Amounts). You should definitely reach out to a planner who knows the ins and outs of IRMAA. A specialist can assist you in orchestrating everything correctly for the best outcome.
Key Takeaway:
HSAs pack a triple tax-saving punch: your contributions, growth, and withdrawals for medical costs are all untaxed. But be careful if you’re nearing Medicare age – stop contributing to your HSA six months before applying to dodge potential tax penalties. Need help navigating? Reach out to an expert who knows the IRMAA ropes.
Delaying Medicare Enrollment for Continued HSA Contributions
The choice to delay your Medicare enrollment is not one to be taken lightly. Before making a decision about delaying Medicare enrollment, you should weigh the implications of your employer’s size and health coverage.
When Might You Consider Delaying Medicare Enrollment?
Delaying Medicare enrollment could be beneficial for those employed by a business with over twenty personnel and possessing an employer-sponsored HDHP. In this case, it may let you continue contributing pre-tax dollars into your Health Savings Account (HSA).
You might ask why? Because once enrolled in any part of Medicare, making contributions to an HSA becomes prohibited by law. This prohibition applies even if other HDHP coverage continues without interruption.
This isn’t just some trivial rule but carries substantial financial implications since HSAs offer triple tax advantages:
- Your contributions lower taxable income,
- Growth within the account is tax-free,
- Distributions used for qualified medical expenses aren’t taxed either.
A key factor driving this decision could also be whether or not you’re collecting Social Security retirement benefits. If yes, then automatic enrollment in Part A kicks off at age 65 which can complicate matters.
To maintain these significant benefits longer while staying on track with legal requirements demands strategic planning around when exactly should one enroll in Medicare – thus stopping HSA contributions six months before doing so helps avoid possible excise taxes on excess amounts contributed during retroactive coverage periods from Part A’s start date backdated to six months before your application (or the first month you were eligible for Medicare, if later).
Let’s put this into perspective with an example. Say John Doe turns 65 on July 1st and has an HSA he’d like to keep contributing to while still working and covered under his employer’s HDHP. If he applies for Social Security retirement benefits or doesn’t delay Part A enrollment upon turning 65, then June becomes the last month that year where contributions can be made without risking excise tax penalties.
Whether you decide to delay enrolling in Medicare depends on many things. Things like whether you’re working, how big your employer is, and what kind of health coverage you already have can all play a part.
Key Takeaway:
Delaying Medicare enrollment can let you keep feeding your HSA with pre-tax dollars, especially if you’re working for a company of over 20 employees and have an employer-sponsored high-deductible health plan. But remember, once on Medicare, contributing to HSAs is no longer allowed by law. So, consider your current job status and the size of your company when making this decision.
The Relationship Between Social Security Retirement Benefits and HSAs
HSAs or Health Savings Accounts offer a way to save for health care costs tax-free. But when you start collecting Social Security retirement benefits, the rules change.
Once you apply for Social Security, Medicare Part A enrollment is triggered automatically, impacting your ability to contribute to an HSA. And that affects your ability to contribute to an HSA.
The Effect of Automatic Enrollment on HSAs
Once you’re receiving Social Security retirement benefits, automatic enrollment in Medicare kicks in. This isn’t necessarily bad – but it has implications if you have an HSA.
This is because enrolling in any part of Medicare makes future contributions to your HSA prohibited by law. It’s crucial then that individuals who want more time contributing pre-tax dollars into their HSAs consider delaying collection of their social security retirement benefits.
Taking Control: Delaying Collection
If continuing contributions to your HSA is important to you and aligns with your healthcare strategy—delaying may be beneficial. By holding off on taking those sweet Social Security checks—you can stay out of the grasp of auto-enrollment into Medicare which lets us continue funding our beloved HSAs.
Consider Your Circumstances Carefully Before Deciding
- Do I possess any other type of medical insurance apart from my high-deductible policy?
- Your medical expenses forecast: How much do I expect spending on healthcare? Could this be covered effectively by maintaining a robustly funded HSA?
Note: It’s not a decision to be taken lightly. Make sure you understand the potential impacts on your financial and healthcare situation before deciding.
The Consequence of Timing
If you decide to delay, remember: timing is everything. To avoid complications with HSA contributions, ensure that Social Security benefits aren’t applied for in the six months prior to enrolling in Medicare.
I apologize, however I don’t have any text for me to revise. Could you please provide the paragraph that needs rewriting?
Key Takeaway:
HSAs offer a tax-free way to save for healthcare, but once you start collecting Social Security benefits and are auto-enrolled in Medicare Part A, contributing to your HSA is off-limits. If an HSA aligns with your health strategy, consider delaying those Social Security checks. This lets you keep pumping pre-tax dollars into your HSA. But remember, it’s important to balance these potential savings against the benefit of receiving social security earlier. So make sure you’re making informed decisions that best suit your individual needs.
Exploring Medicare MSA Plans
Medicare Medical Savings Account (MSA) plans are a unique breed of health coverage. These consumer-directed Medicare Advantage Plans blend elements of a high-deductible health plan with those of a medical savings account.
What are the Eligibility Criteria for MSA Plans?
If you’re unsure whether you meet the criteria to join an MSA Plan, let’s take a look. You must already be enrolled in both Medicare Part A and B. Also, note that certain individuals aren’t eligible to join – including those who have end-stage renal disease (ESRD), unless they meet specific conditions.
The uniqueness about these plans lies within their structure: each year your plan deposits money into your account which is then used towards your healthcare expenses before the deductible is met. So, it’s like having a rainy-day fund specifically for handling unexpected care costs.
How Can You Leave an MSA Plan?
Pulling out from an MSA plan isn’t complicated but does need some planning around timing to avoid any hiccups along the way. The easiest time to leave is during Fall Open Enrollment Period between October 15th and December 7th every calendar year where changes take effect on January 1st next year.
In case you want to drop out at other times during the year, it gets trickier as this would only be possible if there exists qualifying circumstances warranting Special Enrollment Period (SEP). For example, moving out of your plan’s service area or losing current coverage are valid reasons for SEP.
It’s crucial to remember that once you leave an MSA Plan, the account remains with you but won’t receive any more yearly deposits from your former Medicare Advantage Plan. Weigh the consequences before deciding, as utilizing a considerable portion of your funds may have monetary repercussions.
These plans offer a great way to manage health care costs while maintaining flexibility and control over one’s healthcare decisions. But, there’s more.
Key Takeaway:
Medicare MSA Plans blend high-deductible health coverage with a savings account. You need to be enrolled in Medicare Part A and B to qualify, though there are some exceptions. Each year, the plan tucks away money for your healthcare costs into your account. While it’s pretty simple to leave an MSA Plan during Fall Open Enrollment, doing so at other times can be more challenging. But remember this: no matter when you decide to exit the plan, that account remains yours.
Navigating HSAs with Professional Guidance
Gaining the expertise of a professional, such as those at IRMAA Certified Planner , can help you to make the most of your health savings account (HSA) and Medicare coverage. An expert, like those at IRMAA Certified Planner, can provide insights into the best strategies for managing your HSA and Medicare coverage.
Understanding how these accounts work is key to reaping their full benefits. You may know that an HSA is tied to high-deductible health plans, but did you realize contributions are tax-free? And not just when they go in – even distributions used for qualified medical expenses aren’t taxed. This double-tax advantage makes HSAs an excellent tool for healthcare costs planning.
Making Sense of Contributions and Enrollment Dates
A tricky aspect of navigating HSAs involves timing around Medicare enrollment. It’s crucial to remember that enrolling in Medicare Part A or B stops further pre-tax contributions to your HSA. So why does this matter?
If you’re still employed with employer-provided health coverage when turning 65, you might want to delay both collecting social security retirement benefits and signing up for Medicare; allowing continued growth of your tax-advantaged HSA funds.
To avoid unnecessary penalties though, it’s recommended stopping contributing six months before starting any part of Medicare as there’s often retroactive coverage applied from Social Security Administration (SSA).
The Alternative: Migrating Towards MSAs After Retirement
An option after retirement could be exploring a different type of plan: The Medical Savings Account Plan or MSA plan which combines a high deductible insurance policy along with a unique twist on the traditional HSA.
Under this Medicare MSA plan, Medicare deposits money into your account, which you can then use for health care expenses before meeting the high deductible.
The Power of Professional Guidance
It’s not easy to navigate these waters alone, and that’s where professional guidance becomes a lifesaver. It helps with timing contributions to dodge tax penalties and makes sure your healthcare funds are used to the max.
Key Takeaway:
Maximizing your HSA’s potential isn’t a solo mission. With professional guidance, you can understand the tax perks and timing of contributions better, especially when it comes to enrolling in Medicare. Also, consider exploring MSAs after retirement for another twist on health savings.
FAQs in Relation to Medicare and Hsa
Can I have Medicare and an HSA?
Yes, but once you enroll in Medicare, you can’t contribute to your HSA anymore. However, funds already in the account can still be used.
Do I have to stop HSA contributions 6 months before Medicare?
To avoid a tax penalty, halt your HSA contributions at least six months prior to enrolling in Medicare.
Conclusion
Mastering the intersection of Medicare and HSA is like learning a new language. But you’ve done it! You now understand the essentials, from high-deductible health plans to HSAs’ tax advantages.
Now, you’re equipped to navigate decisions around delaying Medicare enrollment for continued HSA contributions. And remember – collecting Social Security retirement benefits can impact this too!
You’ve also unraveled the mystery of Medicare MSA Plans, making sure no stone remains unturned in your journey towards healthcare financial literacy.
Your path through these often confusing corridors just got brighter. Go forth with confidence and make those informed choices that serve your unique needs best!
Table of Contents:
- Understanding Medicare and Health Savings Accounts (HSA)
- The Tax Implications of HSAs
- Delaying Medicare Enrollment for Continued HSA Contributions
- The Relationship Between Social Security Retirement Benefits and HSAs
- Exploring Medicare MSA Plans
- Navigating HSAs with Professional Guidance
- FAQs in Relation to Medicare and Hsa
- Conclusion
Streamlining the Medicare Surcharge Calculation Process.
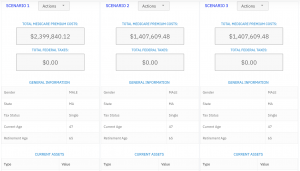
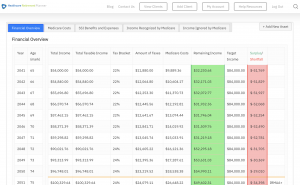
Our Healthcare Retirement Planner software is designed to streamline the retirement planning process for financial professionals. By providing an efficient way to calculate IRMAA costs, our tool helps you save time and focus on other aspects of your clients’ retirement plans.
- Faster calculations: Our software quickly calculates IRMAA costs based on your client’s income and tax filing status, eliminating manual calculations and potential errors.
- User-friendly interface: The intuitive design of our platform makes it easy for financial professionals to input data and generate results with minimal effort.
- Data integration: Seamlessly integrate our calculator into your existing financial planning tools or CRM systems for a more streamlined workflow.
- Easy to Understand Reports: Export reports to easily share with your clients
- Tax and Surcharge Modeling: see how different types of income affects both taxes and your surcharges.
In addition to simplifying the calculation process, using our Healthcare Retirement Planner can also help improve communication between you and your clients. With clear visuals that illustrate how IRMAA costs impact their overall retirement plan, you can effectively convey complex information in an easily digestible format. This enables clients to make informed decisions about their healthcare expenses during retirement while ensuring they are prepared for any potential changes in Medicare premiums due to income fluctuations. To learn more about how our software can benefit both you as a financial professional and your clients’ retirement planning experience, visit the features page. Streamlining retirement planning processes can help financial professionals save time and resources, allowing them to focus on other areas of their clients’ needs. Automated calculation of IRMAA costs is the next step in streamlining this process even further.