Let’s dive straight into the heart of medicare income limits 2024. It’s a topic that can feel like navigating through a dense fog, but clarity awaits for those who persist. Understanding these limits is crucial, as exceeding them can result in an IRMAA surcharge on top of your regular Medicare premiums. Navigating the shifting landscape of this year’s financial adjustments might just surprise you with its impact on your finances. The IRMAA determination is based on your income from two years prior, so it’s important to plan ahead and consider how your retirement income may affect your Medicare costs.
You’ll walk away with an understanding of how gross versus adjusted incomes play pivotal roles in determining your premiums. We’ll shed light on the mysteries of Modified Adjusted Gross Income (MAGI) and its impact on Medicare Part B and D costs. If your MAGI exceeds certain thresholds, you’ll be subject to IRMAA premiums, which can significantly increase your Medicare expenses. Wrapping up, the idea of effortlessly controlling your healthcare spending will suddenly become crystal clear. By staying within the income limits, you can avoid the IRMAA surcharge and keep your Medicare costs more manageable.
This guide promises to equip you with essential knowledge about navigating Medicare costs efficiently, making informed decisions easier than ever before. Additionally, if you qualify for a low-income subsidy, you may be able to get help paying for your Medicare premiums and out-of-pocket costs.
Understanding Medicare Income Limits for 2024
Gross vs. Adjusted Gross Income
When it comes to Medicare in 2024, knowing the difference between gross income and adjusted gross income (AGI) is crucial. Think of your gross income as the total amount you earn before any deductions or taxes are taken out—it’s like the whole pie. Your AGI, on the other hand, is what remains after certain deductions from that pie—like IRA contributions or student loan interest—are subtracted. This distinction matters because your AGI directly influences how much you’ll pay for Medicare premiums. It’s important to keep in mind that there are limits on how much you can earn before your Medicare premiums start to increase.
The sliding scale used by Medicare takes this into account to determine your monthly premiums for Parts B and D. Essentially, as your AGI goes up, so does the cost of your healthcare coverage—a mechanism designed to keep Medicare sustainable while ensuring those who need help most can afford it. Staying within these income limits can help you avoid paying higher IRMAA premiums.
The Role of Modified Adjusted Gross Income
Your modified adjusted gross income (MAGI) plays a pivotal role in setting your Part B and D premiums under Medicare rules for 2024. MAGI adds back certain items to your AGI such as tax-exempt interest earned during the year—think of it as adjusting that slice of pie once more but this time adding some ingredients back in. Your MAGI is what ultimately determines the IRMAA amount you’ll pay on top of your regular Medicare premiums.
MAGI determines where you fall on Medicare’s premium sliding scale. For individuals with higher incomes based on their MAGI levels two years prior—in this case, 2024—their monthly adjustment amounts will be higher compared to those with lower incomes; an effort by Social Security Administration aimed at balancing costs across all beneficiaries without compromising access or quality care provided through plans like medicare advantage or prescription drug coverage.
In essence: know thy MAGI. It could mean significant differences in what one pays annually not just for parts B and D but also affects eligibility thresholds around assistance programs aimed at reducing out-of-pocket expenses related specifically towards prescription drugs within given health care plans available today including medicaid services alongside traditional routes offered via social security measures established long ago yet constantly evolving each taxable year according there needs society faces collectively moving forward together unitedly strong.
Key Takeaway:
Understanding your adjusted gross income (AGI) and modified adjusted gross income (MAGI) is key to predicting your Medicare premiums for 2024. Your AGI affects how much you pay, while your MAGI can alter premium costs and eligibility for help with prescription drugs. Know these terms well to manage healthcare expenses better.
Navigating Medicare Part B Premiums and Deductibles in 2024
If you thought understanding Medicare was as easy as pie, think again. The world of Medicare Part B premiums and deductibles is more like a layered cake, with each tier representing a different aspect of your healthcare costs in 2024. So, grab your fork because we’re about to dig into the delicious details.
Gross vs. Adjusted Gross Income
First off, let’s talk dough—specifically, how much you’ll be dishing out for your standard monthly premium for Medicare Part B enrollees which will hit $174.70 next year. But wait. That’s not all folks; every beneficiary also needs to account for an annual deductible set at $240.
This financial feast depends heavily on what the IRS knows about your income salad—the gross and adjusted kinds that is—and how it affects what you pay for health care coverage under Parts A & D too. Staying within the income limits can help you avoid paying the higher IRMAA premiums that come with exceeding these thresholds.
The Role of Modified Adjusted Gross Income
Your modified adjusted gross income (MAGI) plays chef when determining how much extra seasoning—in this case, money—you need to sprinkle on top of those basic costs through something called income-related monthly adjustment amounts (IRMAA). For high-income beneficiaries, this could mean paying higher premiums based on their MAGI from two years prior.
But here’s where things get spicy: IRMAA isn’t just a flat rate increase across the board but follows a sliding scale based more intricately on one’s earnings bracket—making some pay more than others depending on their reported taxable year earnings to Social Security or Railroad Retirement Board benefits statements via tax returns filed with the Internal Revenue Service (IRS).
Exploring Coverage Options Beyond Original Medicare
Beyond just Parts A & B, there are options like prescription drug coverage through either standalone plans or bundled within certain Medicare Advantage plans. These choices can help manage other expenses related directly towards medications including immunosuppressive drugs necessary post-transplant surgery which are covered under specific conditions by Medicaid services. This helps further reduce out-of-pocket spending annually, regardless of whether you’re enrolled in original Medicare programs separately. They offer various levels among doctor visits, hospital stays etcetera. This proves beneficial over long term periods especially amongst elder populations seeking comprehensive solutions to managing increasing healthcare demands efficiently while still maintaining quality life standards affordably. Hence, it’s essential to make educated choices in order to adeptly tackle the intricacies of contemporary health coverage plans without sacrificing one’s financial stability or overall health and peace of mind. It ensures peace of mind and stability throughout retirement years ahead confidently knowing you’re well-prepared for any unforeseen circumstances that may arise unexpectedly along this journey called life.
Key Takeaway:
Understanding Medicare Part B in 2024 is like slicing through a layered cake, with premiums and deductibles adding to the mix. Your income salad—gross or adjusted—spices up how much you pay. Dive into this financial feast and see how choices beyond Original Medicare can sweeten your healthcare deal, ensuring quality life without breaking the bank.
Insights into Medicare Part A Costs for 2024
If you thought navigating the maze of healthcare costs was as easy as pie, think again. Especially when it comes to Medicare Part A in 2024, where premiums and deductibles take a rollercoaster ride that could make your head spin. Let’s cut through the noise and get straight to what matters most: your wallet.
Voluntary Enrollment: Premiums for Different Coverage Levels
The concept of voluntary enrollment might sound like choosing between chocolate or vanilla ice cream but trust me, it’s slightly more complex with Medicare Part A. For those who haven’t clocked in enough quarters of coverage (less than 40 to be precise), there are two flavors available – one at a reduced rate of $278 per month and another at the full premium cost of $505 monthly. Understanding this difference is vital as it dictates the amount you’ll fork over before ever crossing a hospital’s threshold.
Digging deeper into these numbers reveals why staying informed can save you from future financial headaches. Opting to enroll voluntarily means weighing your work history against potential healthcare needs—a balancing act worthy of any tightrope walker.
Inpatient Hospital Deductible: The First Hurdle
Buckle up; we’re not done yet. Before insurance starts paying its share for hospital stays, enrollees must overcome an initial obstacle—the inpatient hospital deductible which stands tall at $1,632 in 2024. Imagine this as the cover charge at an exclusive club where once inside, some costs are covered but getting through that door? That’s on you.
This upfront cost underscores why planning ahead isn’t just good advice—it’s essential for anyone wanting to keep their finances intact while navigating health challenges that come with age or unexpected conditions requiring hospitalization.
Making Sense Out Of It All With Helpful Resources
Sometimes, the path to understanding cuts through seeking assistance beyond just this write-up. Thankfully, resources like CMS-8083-N documentations provide further insight into changes affecting Medicare costs yearly—including all things related to premiums and deductibles discussed here—giving beneficiaries everything needed for making informed decisions about their health care coverage moving forward into 2024 without surprises lurking around corners.
Tackling information dense topics such as these often leaves many wishing they had paid more attention during math class—or better yet—had someone break down exactly what each term meant without needing a dictionary by their side every step along the way. By understanding key components such as voluntary enrollment options, how different levels affect overall expenses, coupled with comprehensive resources, individuals can make informed decisions that align with their financial and health goals. It’s crucial to stay within the income limits to avoid paying higher IRMAA premiums on top of these Part A costs.
Key Takeaway:
Understanding Medicare Part A’s voluntary enrollment and inpatient hospital deductible for 2024 can save you from financial headaches. Dive into the details to make informed decisions that protect your wallet and health.
Addressing High-Income Beneficiaries’ Concerns in 2024
If you’re a high-income Medicare beneficiary, brace yourself for some changes in 2024. With income-related monthly adjustment amounts (IRMAA) set to impact your costs, it’s crucial to understand how this could affect your wallet.
Understanding IRMAA for Parts B and D
The crux of the matter lies with IRMAA, which adjusts Medicare Part B and D premiums based on your income bracket. Essentially, if you’re earning more, expect to pay higher premiums. By employing a sliding scale method, it’s made sure that individuals with the means to pay more will, thereby bolstering Medicare’s sustainability for everyone. Exceeding the income limits can result in a significant IRMAA surcharge on top of your regular Medicare premiums.
To break it down further: If you fall into the “high-income beneficiaries” category according to the IRS data from two years prior (yes, they look back), get ready to shell out extra dough on top of standard premium rates. For example, as detailed in federal register notices, standard monthly premium rates have been pegged at $174.70 for Part B enrollees in 2024 with an annual deductible of $240. The IRMAA amount you’ll pay is determined by your MAGI from two years ago, so it’s important to plan ahead and consider how your retirement income may affect your Medicare costs.
This might seem like a bummer but remember why IRMAA exists—to ensure everyone pays their fair share towards maintaining our health care system’s viability. And here’s something else—these adjustments aren’t arbitrary; they are meticulously calculated using modified adjusted gross incomes (MAGI). So yes, Uncle Sam uses your tax returns against you—but only fairly so.
Navigating Your Way Through Increased Premiums
Paying higher premiums due to increased earnings may feel like being penalized for success; however let’s flip that perspective. Consider it contributing towards a healthier society where access to quality healthcare isn’t just a privilege but a shared responsibility. By staying within the income limits, you can avoid the IRMAA surcharge and keep your Medicare costs more manageable.
You’re not alone if these increases have got you sweating bullets about financial planning though. Nearly 8% of folks enrolled in Medicare parts B & D grapple with these additional charges annually—that’s millions navigating this boat together. Now while no one enjoys parting ways with hard-earned cash especially when retirement is supposed-to-be all about enjoying life’s later chapters without financial woes—there are silver linings:
- Becoming savvy about managing healthcare expenses now can save headaches down the road.
- Exploring other coverage options beyond Original Medicare such as Medicare Advantage plans or prescription drug coverage might reveal cost-effective pathways previously unconsidered.
Key Takeaway:
High-income Medicare beneficiaries, gear up for 2024. IRMAA will hit your wallet based on what you earn. Paying more helps keep Medicare strong for everyone. Look at it as chipping in for a healthier society and explore ways to manage or offset these extra costs.
Exploring Coverage Options Beyond Original Medicare
If you think Original Medicare covers all your healthcare needs, it’s time for a reality check. Absolutely, Original Medicare covers a decent chunk of the essentials; however, if you’re aiming for thorough protection, there’s quite a bit more to delve into. At this point, it’s essential to explore further into alternatives such as Medicare Advantage schemes and medication coverage plans to ensure thorough protection.
Medicare Prescription Drug Coverage Premiums
First up on our exploration tour are the premiums for Medicare prescription drug coverage. Navigating these waters can feel like decoding a secret message without the cipher—complex but not impossible. The key here is understanding that these premiums vary based on several factors including which plan you choose and your income level. If your income exceeds certain limits, you may be subject to IRMAA premiums on top of your regular Part D premiums.
To give some context, let’s talk about IRMAA (Income-Related Monthly Adjustment Amount). If you’re rolling in dough (kudos to you), expect to pay higher than average premiums for Part D. It operates on a sliding scale—the more you earn, the more you contribute towards your premium costs. But don’t worry; this isn’t designed to break the bank but rather ensure fairness in how much beneficiaries pay based on their financial situation.
Immunosuppressive Drug Coverage
Moving along our journey brings us face-to-face with immunosuppressive drug coverage—a critical aspect if transplantation has been part of your medical history or might be down the road. While original Medicare offers limited assistance here, diving deeper into available plans reveals gold mines worth exploring further at CMS-8085-N. These drugs are pivotal post-transplantation to prevent organ rejection and ensuring they’re covered adequately underlines why looking beyond basic Medicare is essential.
Medicare Advantage Plans: A Closer Look
Last stop? The world of Medicare Advantage plans. Think of them as an all-in-one package deal that bundles Parts A and B with extra goodies like dental or vision benefits—and sometimes even prescription drug coverage thrown into one neat bundle offered by private companies approved by Medicare. So what makes them stand out? For starters, they often come with lower out-of-pocket costs compared to Original Medicare alone plus offer maximum cap limits on annual expenses helping protect against unforeseen high medical bills throughout any given year. Plus, offering insights directly from CMS itself. Keep in mind that if your income exceeds the limits, you may still be subject to IRMAA surcharges even if you have a Medicare Advantage plan.
Key Takeaway:
Think Original Medicare covers everything? Think again. For full coverage, look into Medicare Advantage plans and prescription drug options. Don’t forget, higher income means higher Part D premiums due to IRMAA. Also, explore additional plans for immunosuppressive drugs post-transplantation.
Preparing for Projected Increases in Future Years
Anticipating Changes to Premiums
We, as recipients of Medicare benefits, must vigilantly monitor future trends to grasp how anticipated financial escalations might influence our budgeting strategies. For starters, knowing that the standard premium has been a moving target over the years helps us brace for what’s next. But why should this matter? Well, because these adjustments directly affect your pocketbook. It’s important to stay informed about the income limits and plan ahead to avoid paying higher IRMAA premiums in the future.
The past offers valuable lessons. Looking at years prior, we’ve seen premiums ebb and flow based on various factors including legislative changes and economic conditions. This trend underscores the importance of staying informed and agile with our healthcare budgeting strategies.
Diving into the details, it’s time we delve into the actual figures to fully grasp what’s at stake. While specifics can change year by year, keeping abreast of announcements from reliable sources is key to not being caught off guard. An educated guess today can save you headaches tomorrow as you plan your finances around possible hikes or reductions in costs associated with Medicare coverage.
Navigating through these waters requires more than just a passive glance at yearly updates; it demands active engagement with available resources and possibly seeking expert advice to make well-informed decisions about your healthcare future. Staying within the income limits and planning your retirement income accordingly can help you avoid the IRMAA surcharge and keep your Medicare costs more manageable in the long run.
The Importance of Staying Informed About Projected Increases
We all know that knowledge is power – particularly true when managing health care expenses under Medicare programs. With an eye towards future projections related specifically to standard premiums, beneficiaries have an opportunity not only anticipate but also strategize effectively against potential financial impacts posed by annual rate adjustments.
This foresight isn’t just beneficial—it’s essential for anyone looking forward meticulously manage their budgets without sacrificing quality or access needed medical services. Understanding implications such movements allow individuals tailor savings plans accordingly ensuring they remain covered while minimizing out-of-pocket expenditures whenever possible.
In essence, preparing oneself ahead time by closely monitoring anticipated shifts enables one build resilience amidst fluctuating landscape thus maintaining stability personal finance arena despite external uncertainties surrounding cost structures within realm public insurance offerings like those provided through Social Security Administration mechanisms governing parts A & B along other ancillary benefits therein included. By staying informed and planning ahead, you can ensure that you stay within the income limits and avoid paying the higher IRMAA premiums that come with exceeding these thresholds.
Key Takeaway:
Staying ahead of Medicare premium changes means better financial planning. By watching trends and seeking advice, you can adjust your budget to cover healthcare without breaking the bank.
Enrollment Periods and Coverage Details
Understanding when and how to enroll in Medicare is as crucial as knowing the ABCs. It’s your golden ticket to a world where health care worries are less daunting, assuming you play your cards right during enrollment periods. And let’s be real, who doesn’t want that peace of mind? Enrolling during the right period and choosing the best coverage for your needs can help you stay within the income limits and avoid paying higher IRMAA premiums.
The Calendar Chronicles: Marking Your Enrollment Dates
If there were ever a time to get cozy with your calendar, it’s now. The Initial Enrollment Period (IEP) is like an open door invitation from Medicare but only for 7 months starting three months before you turn 65. Miss this window and you might just find yourself waiting around for the General Enrollment Period (GEP), which opens annually from January 1st through March 31st.
But wait—there’s more. If life throws curveballs at you because let’s face it, life loves doing that, Special Enrollment Periods (SEPs) can come to the rescue allowing changes outside typical timelines due to specific circumstances such as losing coverage or moving.
Diving Into Coverage Particulars
Now onto what feels like deciphering ancient scripts—understanding coverage details across different parts of Medicare. Original Medicare comprises Part A hospital insurance and Part B medical insurance; both have their charm depending on what healthcare adventure awaits.
Here’s something fun: Did you know that while most folks don’t pay a monthly premium for Part A thanks to years of paying taxes, everyone pays a plan premium for Part B? Yes indeed—the standard monthly adjustment ensures we all contribute our fair share towards doctors’ visits among other things.
Navigating Through Premium Adjustments Like a Pro
Sometimes life likes reminding us it has its own plans by throwing adjustments our way based on income levels; hello IRMAA – Income-Related Monthly Adjustment Amount. Whether dealing with Medicare part b premium and deductible costs, understanding these adjustments helps prevent unwelcome surprises in retirement budgets. Knowledge here means power—the power not just survive but thrive under changing financial landscapes within healthcare realms. Staying within the income limits can help you avoid the IRMAA surcharge and keep your costs more manageable.
Becoming acquainted with various enrollment periods plus comprehending coverage nuances isn’t merely about crossing Ts or dotting Is—it shapes experiences within healthcare systems profoundly affecting personal well-being alongside financial stability moving forward into golden years gracefully loaded with wisdom rather than worry about potential mishaps awaiting unpreparedness amidst ever-evolving rules governing Medicare complexities today. Keeping up-to-date is your shield against surprises, guaranteeing a smoother journey forward.
Key Takeaway:
Mark your calendar and know the ABCs of Medicare enrollment to unlock peace of mind. Dive into coverage details, keep an eye on premium adjustments, and stay informed to navigate healthcare in your golden years smoothly.
Strategies for Managing Increased Healthcare Costs
Facing the rising tide of healthcare costs can feel like trying to climb a mountain in flip-flops. Yet, the silver lining is found in savvy maneuvers and resources waiting to be tapped into.
Utilizing Medicare Savings Programs
If you’re wrestling with higher healthcare expenses, diving into savings programs with Medicare might be your first move. These programs are lifesavers for those who qualify, offering a financial cushion that helps pay parts of your Medicare premiums and sometimes even deductibles and copayments. It’s like finding an unexpected treasure chest in your backyard – but instead of gold coins, it’s help from the government paying for crucial health care needs. Taking advantage of these programs can help you stay within the income limits and avoid paying the IRMAA surcharge.
Navigating the intricate world of these supportive schemes, we find major entities like the Social Security Administration and Internal Revenue Service at the helm. They work together to assess eligibility based on income levels reported through tax returns—think of them as gatekeepers deciding who gets access to this valuable aid.
Navigating Tax Implications Wisely
Tax time doesn’t have to be a groan-inducing season if you know how it ties into managing healthcare costs effectively. Your modified adjusted gross income is more than just a number; it dictates what you’ll end up paying for certain Medicare premiums under IRMAA (Income-Related Monthly Adjustment Amount) rules. Planning your retirement income wisely and staying within the income limits can help you avoid the IRMAA surcharge and keep your costs more manageable.
For instance, knowing that daily coinsurance rates will hit $204 in 2024 for extended skilled nursing facility stays underscores why savvy tax planning matters—it directly impacts out-of-pocket expenses tied to health care coverage.
Taking proactive steps now could mean less financial strain later when dealing with inevitable premium adjustments or navigating high-income brackets that require ponying up more cash monthly. By consulting closely with tax professionals familiarized with healthcare-related tax nuances, beneficiaries can position themselves advantageously come April 15th.
Selecting The Right Plan Based On Individual Health Care Needs
Gone are the days when one-size-fits-all solutions sufficed—today’s health care landscape demands personalization down to each individual’s unique circumstances including their preferred doctors’ services or prescription drug needs. Choosing the right plan for your needs can help you stay within the income limits and avoid paying the IRMAA surcharge.
Choosing between Original Medicare versus Advantage Plans becomes akin to selecting between ordering à la carte or going buffet-style: both have merits depending on appetite—in this case, medical services consumption patterns.
Moreover, by engaging proactively when it’s time to enroll, you’re more likely to secure a plan that not only aligns with your health requirements but also proves financially beneficial.
Key Takeaway:
Getting smart about Medicare Savings Programs and tax planning can ease the burden of rising healthcare costs. Dive into these options early to save on premiums, deductibles, and copays. Choose your plan wisely based on personal health needs for more tailored coverage.
Key Statistics & Facts from Recent Research
Did you know that in 2024, the daily coinsurance for days 21 through 100 of extended care services in a skilled nursing facility will be $204.00? That’s right, and it’s not just an arbitrary number pulled out of thin air. This figure is part of a broader framework designed to manage Medicare costs effectively while ensuring beneficiaries receive the care they need.
Speaking of managing costs, let’s talk about IRMAA – the Income-Related Monthly Adjustment Amounts. Roughly 8 percent of folks enrolled in Medicare Part B and D find themselves navigating these extra charges due to their higher income brackets. If you’re wondering how this might affect you or someone you love, keep reading because understanding these nuances can save some serious cash down the line. Staying within the income limits can help you avoid paying the higher IRMAA premiums.
Gross vs. Adjusted Gross Income
The distinction between gross and adjusted gross income (AGI) isn’t just tax jargon; it plays a crucial role in determining your Medicare premiums too. Your AGI includes all taxable income minus specific deductions like student loan interest or contributions to retirement accounts—pretty important stuff when considering potential impacts on your healthcare expenses. Keeping your AGI within the income limits can help you avoid the IRMAA surcharge and keep your Medicare costs more manageable.
This calculation directly influences what’s known as Modified Adjusted Gross Income (MAGI), which then determines whether or not those dreaded IRMAA surcharges apply to your situation—a key consideration for anyone trying to navigate future health care planning efficiently.
The Role of Modified Adjusted Gross Income
MAGI is essentially AGI with some additions back into the mix—it’s what Medicare uses to decide if you’ll pay standard rates for Part B and D coverage or pony up more via IRMAA based on higher earnings levels set by federal guidelines each year—an aspect that underscores why keeping tabs on these changes matters greatly for personal financial planning related to health care expenditures.
To get a grip on specifics surrounding adjustments made across various parts of the program next year, take a peek at recent announcements detailed within CMS-8085-N. It outlines everything from premium hikes tied closely with inflation rates through nuanced shifts affecting certain drug coverages—all pivotal info aimed at helping beneficiaries strategize effectively around rising medical expenses moving forward without unwelcome surprises derailing budgetary considerations along the way. Staying within the income limits and planning your retirement income accordingly can help you avoid the IRMAA surcharge and keep your Medicare costs more manageable.
Beyond cold hard stats, however, lies a deeper narrative centered upon real people grappling with day-to-day challenges presented by a complex system. This ultimately drives ongoing discussions around reform possibilities aiming to better serve the community at large. Regardless of their financial standing, each person is entitled to a fair chance at securing consistent and just access to superior resources.
Key Takeaway:
Knowing the 2024 coinsurance rates and how IRMAA affects Medicare Part B and D due to income can save you money. Understanding your AGI’s role in this process is key for smart health care planning, helping avoid extra costs.
Conclusion
Navigating medicare income limits 2024 can feel like a maze. But, you’ve got the map now. Understanding gross versus adjusted incomes matters. It shapes how much you pay for Medicare Part B and D. MAGI plays a big role too. It decides your premium costs based on your income bracket. Staying within the income limits can help you avoid paying the higher IRMAA premiums. Knowing when to enroll is crucial. So is picking the right plan for your healthcare needs. Keep up with shifts in costs and out-of-pocket expenses to smartly handle your finances. With the knowledge from this article, making choices about Medicare will seem less intimidating, as it equips you with the necessary understanding to simplify these decisions annually. By planning ahead and considering how your retirement income may affect your Medicare costs, you can stay within the limits and avoid the IRMAA surcharge, keeping your healthcare expenses more manageable in the long run.
Table of Contents:
- Understanding Medicare Income Limits for 2024
- Navigating Medicare Part B Premiums and Deductibles in 2024
- Insights into Medicare Part A Costs for 2024
- Addressing High-Income Beneficiaries’ Concerns in 2024
- Exploring Coverage Options Beyond Original Medicare
- Preparing for Projected Increases in Future Years
- Enrollment Periods and Coverage Details
- Strategies for Managing Increased Healthcare Costs
- Key Statistics & Facts from Recent Research
- Conclusion
Streamlining the Medicare Surcharge Calculation Process.
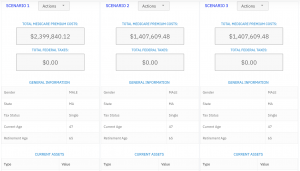
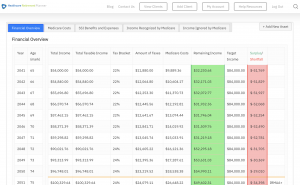
Our Healthcare Retirement Planner software is designed to streamline the retirement planning process for financial professionals. By providing an efficient way to calculate IRMAA costs, our tool helps you save time and focus on other aspects of your clients’ retirement plans.
- Faster calculations: Our software quickly calculates IRMAA costs based on your client’s income and tax filing status, eliminating manual calculations and potential errors.
- User-friendly interface: The intuitive design of our platform makes it easy for financial professionals to input data and generate results with minimal effort.
- Data integration: Seamlessly integrate our calculator into your existing financial planning tools or CRM systems for a more streamlined workflow.
- Easy to Understand Reports: Export reports to easily share with your clients
- Tax and Surcharge Modeling: see how different types of income affects both taxes and your surcharges.
In addition to simplifying the calculation process, using our Healthcare Retirement Planner can also help improve communication between you and your clients. With clear visuals that illustrate how IRMAA costs impact their overall retirement plan, you can effectively convey complex information in an easily digestible format. This enables clients to make informed decisions about their healthcare expenses during retirement while ensuring they are prepared for any potential changes in Medicare premiums due to income fluctuations. To learn more about how our software can benefit both you as a financial professional and your clients’ retirement planning experience, visit the features page. Streamlining retirement planning processes can help financial professionals save time and resources, allowing them to focus on other areas of their clients’ needs. Automated calculation of IRMAA costs is the next step in streamlining this process even further.